Medial Tibial Stress Syndrome (MTSS), commonly referred to as shin splints, is one of the most common lower leg injuries in sports and frequently affects active individuals. Shin splints can be an annoying, frustrating injury to be dealing with and often mean you need to cool it from your activities for a while to rehabilitate.

prevalence
Incidence varies between 4-35% in athletic and military population and as much as 50% of all lower leg running injuries.
anatomy
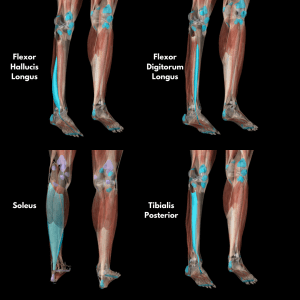
The soleus muscle is involved in MTSS and the muscles that control foot/ankle pronation i.e. tibialis posterior, flexor hallicus longus, and flexor digitorum longus. See the photos below highlighting these muscles!
etiology
MTSS is a consequence of repetitive stress imposed by impact forces.
It is theorized that the cortical bone of the tibia suffers microtrauma which develops over a period of time and eventually results in a periosteal (fascia surrounding the outer surface of bone) soft tissue reaction in the region of the microtrauma. Another theory is that muscle fiber traction from the soleus, tibialis posterior, flexor digitorum, and flexor hallicus muscles, all attaching to the tibia, cause periostitis which may or may not lead to cortical bone microtrauma.
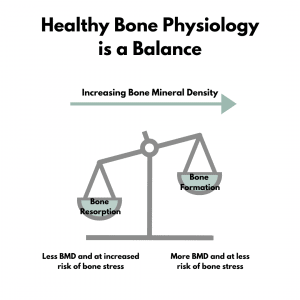
Due to the lack of histology studies which provide evidence that MTSS is caused by periostitis, the more commonly accepted theory is that MTSS is caused by bony resorption that outpaces bone formation of the tibial cortex. Several studies have found evidence for this overload adaptation of the cortex i.e. MRI, CT, and DEXA imaging.
MTSS = Load > Tissue Capacity
pathophysiology
Normally, bones can detect and repair small microdamage caused by strains that stay below the microdamage threshold. Strains above the threshold can cause enough microdamage to escape repair. Overtime, this repeated loading of the tibia through impact forces can cause overloading of the remodelling capabilities of the tibia.
In patients with MTSS, low regional tibial bone density has been found compared with healthy athletes. Bone density in the mid-to-distal tibia measured by DEXA was 23% less in patients with MTSS. On a good note – athletes are able to regain bone density values comparable to healthy norms overtime.
signs & symptoms
MTSS is an overuse injury which characteristically presents with (1) diffuse pain, (2) pain located along the anteromedial or posteromedial border of the tibia over a length of at least 5 cm (usually the middle or distal thirds), and (3) pain is triggered by activity.
Initially symptoms are present at the start of an activity and subside with continued exercise. Later on as this injury progresses, the pain continues to be present during the entire activity. If symptoms worsen, the pain can be felt even after the activity ceases.
differential diagnosis
- Exertional compartment syndrome: closely mimics MTSS due to the location of symptoms and activity related pain, however, with this injury there are complaints of cramping, burning, aching and tightness during exercise. Sometimes may present with neurological symptoms such as sensory abnormalities. No pain at rest to palpate, but during exercise it becomes painful and disappears quickly after exercise.
- Stress fractures: it is challenging to differentiate between MTSS and stress fractures. Even radiographic imaging can produce false negatives 26-52% of the time. Pain with stress fractures is more localized pain versus the diffuse pain felt with MTSS. Pain at night and pain on percussion are usually not present with MTSS and may be present with stress fracture. There is some thought that stress fracture may be on the continuum of MTSS injury but that has not been confirmed as of yet in the research.
risk factors
Reinking et al concluded that these 5 risk factors showed high evidence for increased risk for the occurrence of MTSS:
- Female sex
- Higher weight
- Higher navicular drop
- Previous running injury (any previous running injury, not just shin splints)
- Greater hip external rotation with hip flexed (we’re looking at you more hypermobile peeps!)
Other proposed risk factors include: increased foot pronation, increased varus tendency of the forefoot/hindfoot, abrupt increase in training intensity, training on hard or inclined surfaces, inadequate shoes, and inadequate calcium intake. Maximum velocity of pronation had a greater correlation in those with MTSS than did pronation alone.
treatment
Clinical relevance of these risk factors contributing to MTSS treatment:
- Increase strength and endurance of the soleus muscle
- Control over-pronation which may alleviate some stress on the medial fascial attachment of these muscles
- Promote adequate shock absorption via insoles, new shoes, and maintenance of proper foot biomechanics
- Working with your healthcare provider or coach to include cross-training weekly that unloads the tibia and allows the bone remodelling response to catch up
The most promising support for the prevention of MTSS includes:
- Shock-absorbing shoes
- Pronation control insoles (specifically controlling navicular drop)
- Graduated running programs.
Running shoe mileage may also have similar effects on shock absorption, therefore it is suggested that running shoes should be replaced when worn between 300-600 miles, depending on body weight, training surface, and running style.
Weak or fatigued muscles cannot absorb shock and dissipate ground reaction forces as well as strong, rested muscles, therefore we also suggest having good overall strength of most of your major lower body muscle groups is also a great idea for helping reduce bone injury.
Conservative therapy such as chiropractic, physiotherapy, and massage therapy are recommended over more invasive interventions for the treatment of MTSS. Interventions include: strengthening exercises for soleus and tib post, stretching for sore/tight muscles, acupuncture, taping, and manual therapy techniques like joint mobilization, massage, and active release techniques (ART).
Custom orthotics are also one of many conservative treatment options available for treating MTSS for those with over-pronation or navicular drop. These devices are designed to restore functional capacity to the foot, control abnormal motion, reduce stress on soft tissues and help alleviate pressure in the lower leg. A registered chiropodist can perform an evaluation of your feet and take a cast moulding to manufacture a custom orthotic based on your individual needs.
A combination of manual therapy, education and strength + conditioning should be established with your clinician. Your rehab should also be specific to YOU! Our clinicians at Function101 can determine which risk factors may be driving your pain and help you move forward.
101
- soleus/deep tib post compartment self-massage (gentle!)
- lateral step down (small step)
- seated calf raise with ball squeeze
- monster walk (band around feet)
201
- y excursion balance on airex pad
- standing calf raise with ball squeeze
- standing hip abduction (banded)
301
- step down curtsy lunge
- single leg calf raise (medial bias)
- single leg depth jump
Follow us on instagram @function101locke for more educational content!
References:
Craig DI. Medial Tibial Stress Syndrome: Evidenced-Based Prevention. Journal of Athletic Training. 2008;43(3):316-318
Moen MH et al. Medial Tibial Stress Syndrome: A Critical Review. Sports Med. 2009:39(7): 523-546
Reinking MF et al. Medial Tibial Stress Syndrome in Active Individuals: A Systematic Review and Meta-analysis of Risk Factors. Physical Therapy. 2017; 9(3)



