The Temporal Mandibular Joint, also known as TMJ, is the joint connecting your jawbone to your skull. You have one joint on each side of your jaw. TMJ disorders can cause pain in your jaw joint and in the muscles that control jaw movement. Onset of symptoms can be slow or quick to develop with worsening pain typically with activities using the jaw i.e. eating, talking, singing, yawning etc. Patients with TMJ disorders frequently present to us as health care professionals for diagnosis and treatment, and we’re here to help!
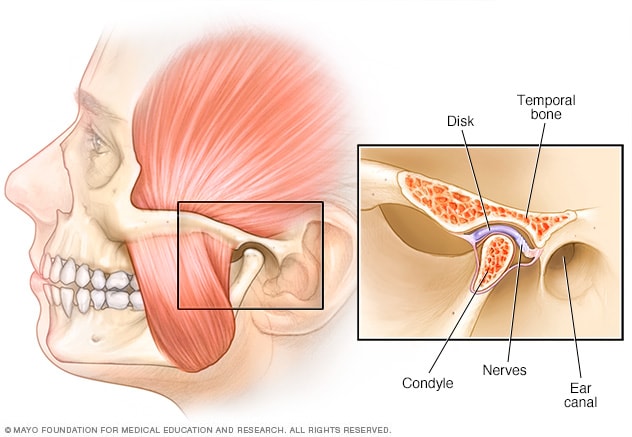
Anatomy
- The TMJ is a complex synovial joint, which has an intra-articular disc lined with fibrous connective tissue
- The joint is between the Mandibular condyles (jaw) and mandibular fossa + articular eminence (temporal bone of the face)
- The intra-articular disc is made up of thick fibrous tissue held in place by ligaments/connective tissue as well as being attached to a muscle called the lateral pterygoid, which helps with the function of opening and closing the jaw to keep disc in place
Biomechanics
- There are 3 Degrees of Freedom/movements that the TMJ can perform: open/close, protrusion/retrusion (movement forward and backwards), laterotrusion (movement side to side)
- Maximum tension on the joint occurs during maximal opening when the ligaments are taut. Also, maximum tension occurs when the teeth are fixed together and jaw is in a clenched position. **Being in a maximum tension position long standing increases the pressure and depletes the absorbed fluid.
- Rest position is when there is about 1-3mm of opening between the teeth and the tongue is resting on the soft palette (tongue resting behind upper teeth and on the dome area in your mouth, such as during clucking) **This resting position allows articular surfaces to absorb fluid.
- Deviations or changes to the opening pattern in the form of a “c curve” or “s curve” can be seen with dysfunctions such as capsulitis or arthrosis. **Deviations can prevent functional opening.
So, what is TMJ disorder?
Patients seeking out treatment for TMJ disorder most often complain of joint pain/myofascial pain. They may experience pain alone, or may present with pain which limits the range of motion of the jaw, most often limitations in opening.
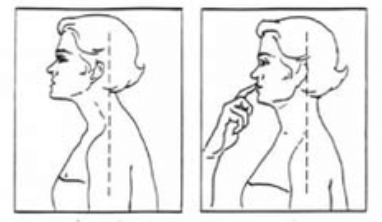
The Rocabado model on caustion of TMJ disorder involves a cascade of events beginning with forward head posture. This posture change leads to shortening of the suboccipital muscles and sternocleidomastoid, resulting in compensatory elevation and forward rotation of the shoulder complex. The altered head and shoulder position leads to increased tension of suprahyoid and infrahyoid muscles, which changes the resting position of mandible, tongue and hyoid. With an altered resting position of the jaw, this now changes the contact between your upper and lower teeth from their ideal position, leading to increased central nervous system input to increase muscle bracing and ultimately to increased stress on the TMJ.
Additionally, psychological and physical stress can influence the central nervous system control, stimulating hyperactivity of jaw and neck muscles. Prolonged muscle tension and increased stress on the TMJ changes the fluid flow in the joint, impacting the lubrication between the articular surfaces, which is important for overall joint health.
Another condition that may occur in patients seeking out care for TMJ disorder is called “Internal Derangement”. This condition involves the articular disc becoming displaced from its original position the condylar head. Most commonly being disc displacement anteriorly with reduction. Patients may present with clicking, snapping, and or a popping noise with or without intermittent locking. Range of motion is not limited, however, movements may not be as smooth as a normal TMJ. Disc displacement can also occur without reduction which may limit someones ability to open their mouth fully. In majority of internal derangements, the prognosis is good, particularly with conservative care. It is rare to need surgery.
On your initial assessment, your physiotherapist or chiropractor will listen to your story and take a detailed health history, all of which will guide a thorough movement assessment.
Joint specific questions
- Location of pain at TMJ region
- May complain of pain during: opening/ closing mouth, eating, chewing, yawning, swallowing, speaking
- Associated symptoms include: ear symptoms (ringing, stuffiness, dizziness, loss of hearing acuity), cervical spine and headaches, eye pain, ANS,
- May complain of pins and needles/numbness of face, palate, gum/tongue
- May experience joint noise (clicking – may be reproducible, crepitus)
- May experience joint locking; truly locked, can they unlock it or any trauma that led to locking
- May have restricted range of motion
- Food/chewing habits, grinding teeth, clenching jaw, mouth breathing, biting nails/objects, smoking, chewing gum, singing/musical instruments, sleep posture (hand cradle under chin)
- Dental signs and symptoms and dental history (orthodontics, dentures, missing teeth, retainer or night guard)
Objective assessment
- Cervical spine range of motion (spinal findings may refer pain to the TMJ region)
- General posture
- Facial posture (observe facial symmetry)
- Breathing pattern (mouth, nose, apical, diaphragm)
- TMJ Range of motion: Normal opening for adult =50-60mm; restricted opening diagnosed less than 40mm; looking for symmetry with lateral deviations
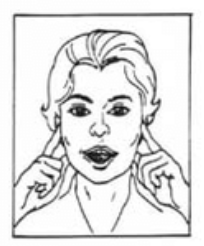
- Palpate extra oral muscles (masseter -clench teeth, temporalis – clench jaw, medial pterygoid – palpate from inner aspect of angle of jaw)
- Palpate infra oral muscles (medial pterygoid- palpate from medial aspect of Mandibular Ramus; and lateral pterygoid)
- Passive joint glides (caudal distraction, distraction with anterior/posterior glide, lateral/medial translation, anteroinferior translation)
- Resisted tests (opening, closing, protrusion, retrusion, lateral deviations)
How can we help?

Management of TMJ disorder should be an individualized approach based on your main complaints and the contributing factors leading to this pain experience. Treatment usually consists of education, manual therapy and exercise. Your therapist may also suggest acupuncture for pain management.
Education: Education is always big part of your recovery journey. Your therapist will educate you on the natural course of TMJ disorder being transient, self-limiting, and frequently without long term effects. Joint sounds may persist, but as long as they are neither painful nor inhibiting to your function, they are clinically not relevant. Load management by limiting the use of your jaw, relaxing the jaw muscles, limiting habits such as refraining from biting your nails or chewing on objects.
Manual Therapy: Therapists may use manual therapy (active release technique, soft tissue therapy, joint mobilizations) in conjunction with exercise prescription. Whether you are visiting chiropractic, physiotherapy, or massage therapy, manual therapy performed by a skilled therapist can help improve joint lubrication, assist the mandible in its available ranges of motion, and reduce muscle tension. Manual therapy techniques may be performed intra orally using gloves and can be quite effective in relaxing hyperactive muscles and improving joint glides. Extra oral techniques can also be performed for those who cannot open their mouth fully or are not comfortable with the intra oral treatment.
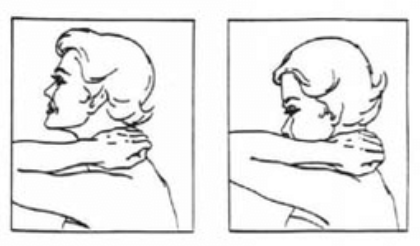
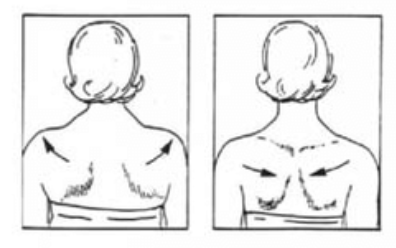
Exercise: Exercise therapy is also a critical component of recovery to improve posture awareness, joint mechanics, and coordination. For patients who experience bothersome joint locking, exercises for range of motion can be done to improve joint lubrication in an effort to decrease the frequency of joint locking. This can be done by moving the mandible fully through all directions of movement (open, protrusive, retrusive, and laterotrusive) after capturing the disc. Coordination and proprioception exercises should be performed without allowing the disc to re-displace. Rocabado 6 x 6: From the Rocobado model, these exercises are prescribed 6 repetitions x 6 sets per day; (1) 6 deep breaths with the tongue in its resting position (soft palette behind the teeth); (2) TMJ rotation control, (3) rhythmic stabilization technique, (4) liberation of the cervical joint in self cervical distraction with cradle of neck; (5) axial extension of the cervical spine and (6) shoulder girdle retraction.

Acupuncture: Clinicians trained in acupuncture may use this modality in their treatment sessions to reduce pain in patients with TMJ disorder. Our team of chiropractors and physiotherapists are trained in acupuncture ranging from dry needling, electroacupuncture, and traditional methods.
If you are suffering from jaw pain and this blog post sounds like you, Book online with one of our chiro’s or physio’s today and follow us on instagram @function101locke for more educational content!



